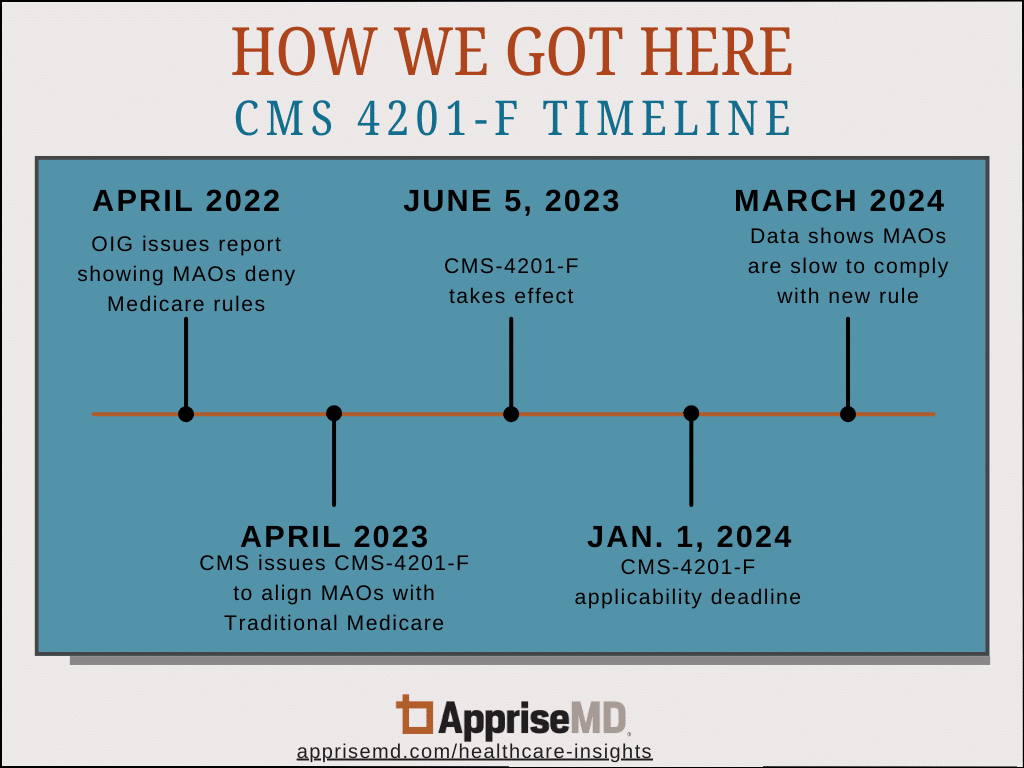
Arising from concerns that the Medicare Advantage Organizations (MAOs) were delaying and denying services and reimbursement, the Centers for Medicare and Medicaid Services (CMS) implemented 4201-F at the beginning of 2024. This rule was initiated after the publication of a report in April 2022 by the Office of the Inspector General (OIG), a division of the United States Department of Health and Human Services (HHS). The OIG’s specific findings pertained to the “circumstances under which MAOs denied requests that met Medicare coverage rules and the MAO billing rules provide an opportunity for improvement to ensure that Medicare Advantage (MA) beneficiaries have timely access to all necessary health care services, and that providers are paid appropriately.” CMS concurred with the report’s three recommendations and issued CMS-4201-F in April 2023.
The 2024 CMS final rule intends to provide much-needed relief to hospitals and health systems by requiring MA plans to follow certain rules that previously only applied to Traditional Medicare patients for inpatient admissions. Specifically, the final rule set the expectation that MA plans must follow the Two-Midnight rule, the CMS inpatient-only list and the caseby-case exceptions. The rule’s objective aims for MA inpatient coverage decisions to be treated the same as Traditional Medicare inpatient coverage decisions.
Two months into 2024 though, our data suggests that the MAOs are not yet complying. Read our findings in our new white paper, Medicare Advantage and the Two-Midnight Rule: 2024 Findings.