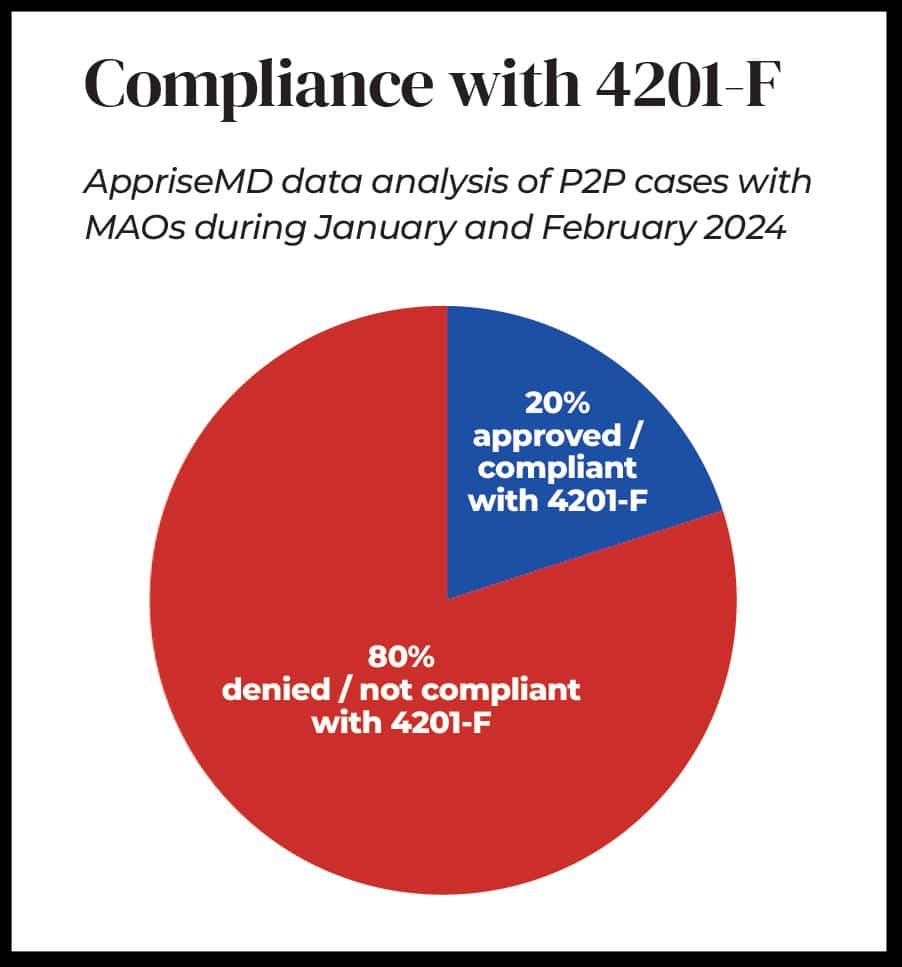
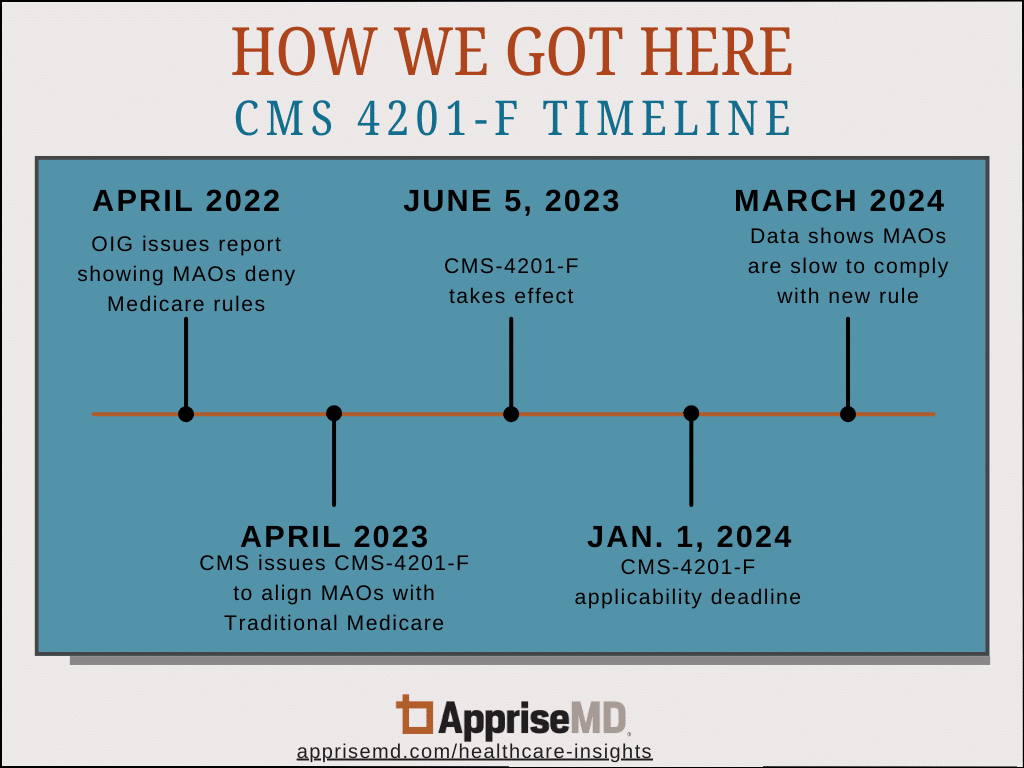
Case Study: Medical Necessity and Reasonable Expectations
CLINICAL SUMMARY: A 73-year-old patient’s primary care doctor sent her to the Emergency Department (ED) after multiple labs taken for continuing chest pains showed abnormal results. The patient, who had been suffering chest pain for more than a week and who was taking nitroglycerin, had a stent placed in April. The patient had an extensive […]
Case Study: Medical Necessity and Reasonable Expectations Read More »