AppriseMD Insights
Understanding Aetna’s New Level of Severity Inpatient Payment Policy
Are Rising Healthcare Costs And Increasing Denial Rates Impacting Your Hospital’s Revenue?
Physician Advisors: Specialists For Your Utilization Management Team
Hospitals Should File A Complaint When Medicare Advantage Plans Do Not Follow Two-Midnight Rule
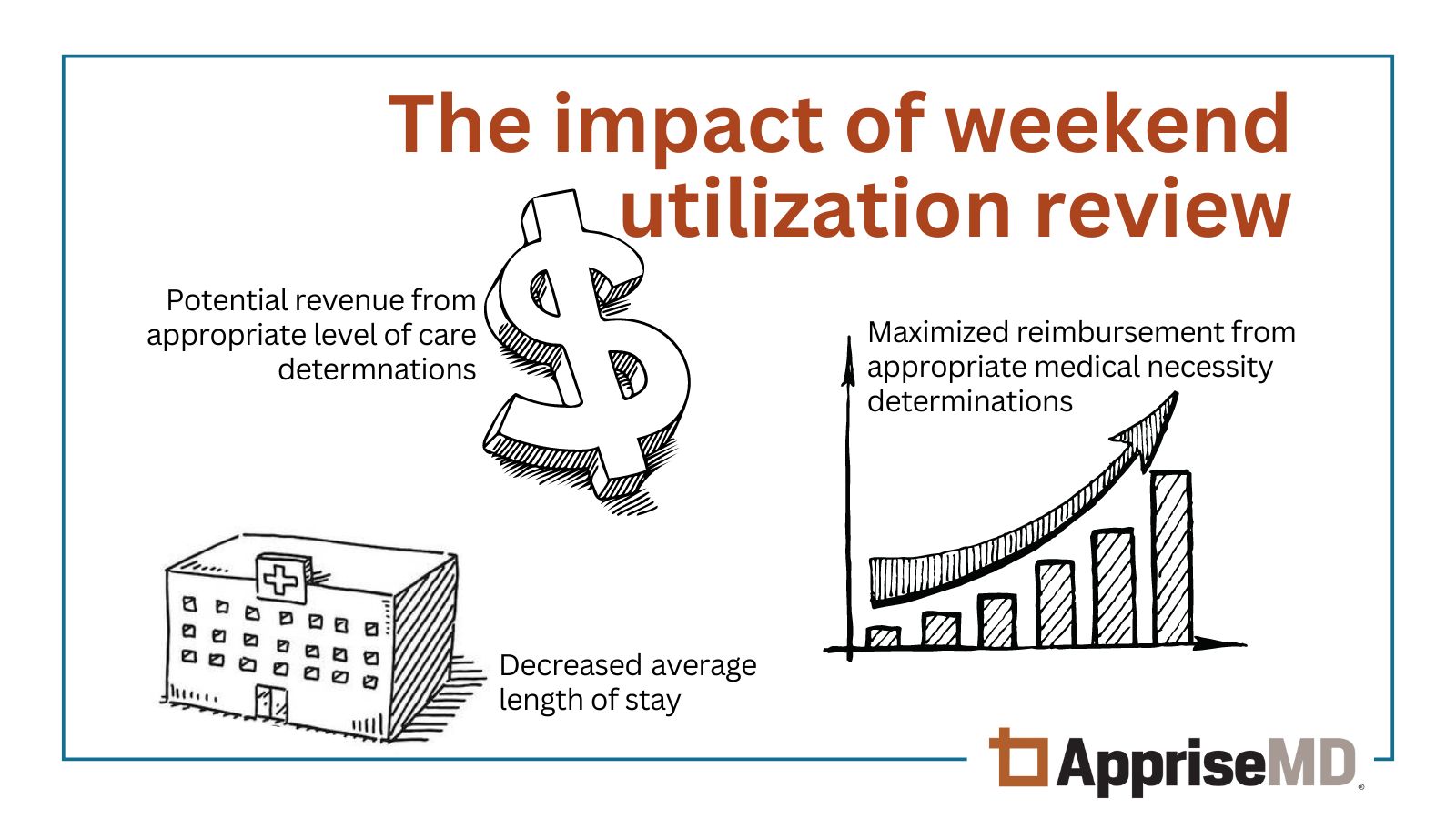
The Financial Impact of Weekend Utilization Review
Payers, Artificial Intelligence and Revenue Cycle
More from the AppriseMD Library
Additional News to Note
Legislation
A law restricting health insurance companies from using AI to alter provider codes that otherwise change the provider’s clinical judgment was introduced in New Hampshire.
→ Read about the proposed legislation.
Texas joins California in looking at how payers are using AI to deny claims.
Outlook
Medicare Advantage enrollment is expected to decrease in 2026.
While the MA market share grew in 2025, it was not as much as anticipated. The lower than projected enrollment growth stems from several factors, one of which includes provider pushbacks. This is not surprising given the prevalence of claim denials, prior authorization requirements and reimbursement challenges that have plagued hospitals and physicians.
→ Read more about MA enrollment expectations in 2026.
AHA & AMA
AppriseMD applauds the American Medical Association for the launch of the Center for Digital Health and AI, "a new endeavor created to put physicians at the center of shaping, guiding, and implementing technologies transforming medicine."
The American Hospital Association (AHA) commended CMS for initiating steps to expand oversight of the 2026 Medicare Advantage (MA) plans last month.
Download AHA fact sheet "Improving Access to Care for MA Beneficiaries."
According to the AHA, hospitals continue to encounter obstacles from insurer policies, negatively impacting patient care and costs.
Stay Apprised
Sign up to receive case studies and papers from AppriseMD.
PRESS RELEASES
Press Inquiry
For more information, contact:
Barbara Esteves-Moore
bestevesmoore@apprisemd.com or info@apprisemd.com