WHITE PAPER
Should hospitals pursue appeals of medicare denials?
Hospital executives and case review managers should soon see the back-logged appeals process speed up for denied Medicare claims. That means hospitals now have one less reason not to pursue appeals of Medicare denials.
According to attorney Knicole C. Emanual, writing for RACmonitor, The Centers for Medicare and Medicaid Services (CMS) has given The Office of Medicare Hearings and Appeals (OMHA) enough new funding to hire 70 additional administrative law judges. These new judges will be charged with hearing the backlog of appeals cases that up until now had a 4-6-year waiting period. Emanual writes, “OMHA now has the capacity to hear and render decisions for approximately 300,000 appeals per year,” which she said was higher than the number of appeals being filed.1
“OMHA was created by the Medicare Modernization Act of 2003 to simplify the appeals process and make it more efficient. During an appeal, an OMHA Administrative Law Judge or attorney adjudicator conducts a new ("de novo") review of an appellant's case and issues a decision based on the facts and the law.”4
This is good news for hospitals who have been waiting on appeals or not even filing appeals due to the backlog. Case in point is a client hospital who recently went before an administrative law judge (ALJ) to appeal a case that is nearly six years old. Why would a hospital spend the time and money to take an appeal all the way to an administrative law judge? In this case, it is because the hospital, and AppriseMD in its review of the case, feels it has a strong case for overturning the denial and ultimately getting paid for the services rendered.
And Emanual agrees. Speaking with AppriseMD, she said more cases need to be appealed because the success rate is over 75% at the ALJ level. Emanual’s numbers were backed up during a Senate Hearing on the backlog of cases several years ago. The Hearing records from April 28, 2015 discussed the matter, “Additionally, large portions of the initial payment determinations are reversed on appeal. The HHS Office of Inspector General reported that, of the 41,000 appeals that providers made to administrative law judges in fiscal year 2010, over 60 percent were partially or fully favorable to the defendant. Such a high rate of reversals raises questions about how the initial decisions are being made and whether providers and beneficiaries are facing undue burdens on the front end. On the other hand, we need to recognize that ALJs have more flexibility in their decision-making than Medicare contractors do.”2
Emanual said denials are often returned to hospitals with amorphous reasons – something like, “the documents don’t support this level of care.” If hospitals do not push to overturn the denial or go through the appeals process, they miss the opportunity for discovery, which considers the full history of the case including a patient’s full medical history. They also do not get paid.
Administrative law judges are familiar with the Medicare and Medicaid cases they are hearing as it is their sole assignment. But even though the judges are familiar with the medical cases in front of them, hospitals are wise to have an attorney present during proceedings because although held to a different standard than a “typical” court case, it is still a legal case. Physicians and case managers may feel more comfortable with their hospital’s legal counsel on the call, if anything, to help with the process and flow.
Tips for preparing for an ALJ appeal hearing:
- Assign a team to handle appeals as the process is long and takes a significant amount of prep time. In preparation for a recent ALJ hearing, AppriseMD worked with a hospital client’s director of utilization management and senior appeals level nurse auditor to review all medical records including the original operation for which payment was denied by Medicare. They reviewed the patient history, the details of the hospitalization, the surgical procedure, how patient faired after procedure, and the discharge process. They then reviewed all the denials that lead up to the ALJ appeal.
- Have a hospital attorney at least present at an appearance in front of an ALJ. It is a legal hearing and clinical staff who handle the actual cases in the hospital need the support of an attorney who understands what they don’t about the legal proceedings, arguments, and terminology.
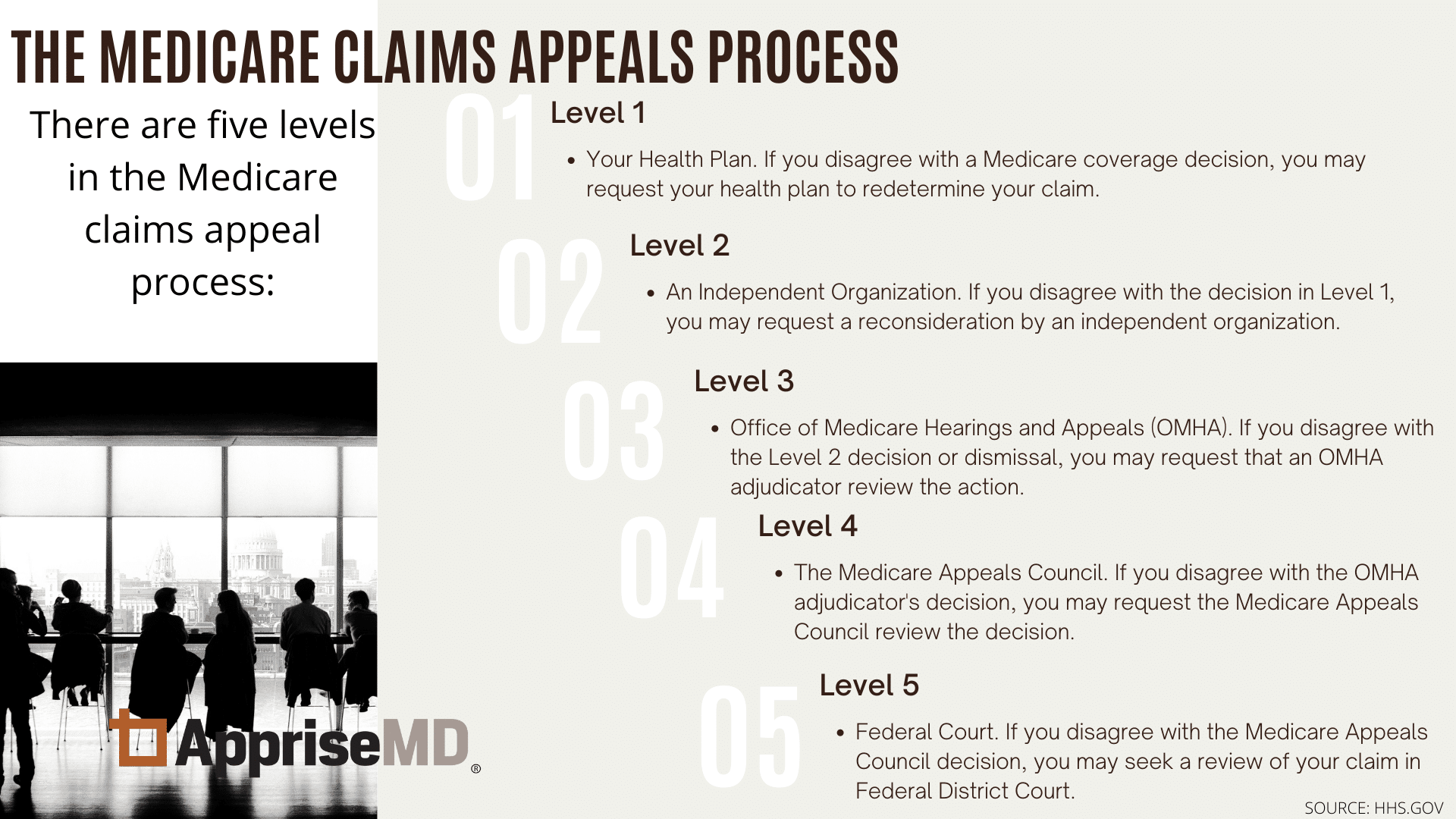
- Familiarize yourself with the OMHA process and levels of appeal.
- Be prepared with a plan for how far you will take each appeal.
Why would a hospital continue to move through this appeals process?
Financial reasons are part of the objective in appealing denied cases; hospital are due the money. In 2015, CMS paid 1,900 hospitals $1.3 billion in a deal to clear out Medicare payment appeals.5 If a hospital and UR team feels they are rightly due payment, the hospital should appeal the case. Does there get to be a point where the ROI is not worth it? Maybe. But the bigger issue is being paid for legitimate services rendered, especially considering the great number of denials coming through government auditors. If a hospital determines a denial is wrong, appealing a denial is appropriate. In the case involving AppriseMD, the hospital was so sure it was correct in its level of care and the reasons for the denial from the RACs made such little sense, the hospital thought it was in its best interest to continue to appeal. The process has taken years and finally went to an ALJ this spring. A decision is expected within 90 days.
Don’t let a denial get to this point
Another strategy for hospitals – perhaps a much more palatable strategy -- is to not let denials even get to the appeals process. By conducting Peer-to-Peer reviews with commercial carriers for Managed Medicare patients or making a RAC Discussion Request within 30 days of a traditional Medicare denial to seek a reversal of the denial, the entire appeals process can be avoided.
The P2P process is not an appeal; it is a reconsideration of a denial, therefore, if a hospital can get a denial overturned the entire drawn-out appeals goes away. In addition, a commercial denial reversed immediately is as if it never happened in terms of payment. Although the P2P process is not always available to a hospital, when it is, there is very little downside to pursuing it.
For traditional Medicare denials, RAC offers an opportunity within 30 days of its denial for a “Discussion Request” which consists of a Discussion Request Form that asks for “evidence to support why you feel the services you provided are covered by Medicare and were properly coded and correctly billed,” according to a RAC Results Letter. There is also an option available to have a physician who is employed by the provider speak to the auditor’s medical director. However, if the window for the Discussion Request is missed or the findings are upheld, the case would roll into the Level One formal appeal as the next opportunity for the hospital to appeal.
CASE SAMPLEAppriseMD and a client hospital recently argued a case in front of an Administrative Law Judge. The case involved a traditional Medicare patient who underwent a total knee replacement. The inpatient services were denied by a Recovery Audit Contractor (RAC) hired by CMS to make sure hospitals are paid appropriately through Medicare Part A. Two different RAC auditors, first WPS and then Maximus, reviewed the case and denied the hospital payment of the inpatient procedure. At the time of the procedure, CMS rules (guided by its Inpatient Only List) said a knee replacement had to be an in-patent procedure. The hospital followed those guidelines and performed the procedure as an inpatient hospital stay. Both auditors denied the inpatient stay saying it was not appropriate because patient did not spend two midnights in the hospitals. There is a separate hospitalization rule, appropriately called the two-midnight rule, which says that a patient physically must cross two midnights to be considered an inpatient stay. There are some exceptions to the two-midnight rule and one of those exceptions is if a patient is admitted to the hospital for a procedure that is on the CMS Inpatient Only List. In other words, if you have this procedure and you don’t cross two midnights, you’re still inpatient. WPS and Maximus both said the patient did not cross two midnights and therefore should not be paid as inpatient. In presenting the case to the ALJ, AppriseMD summarized the case, giving a full medical history of the 67-year-old patient and then reviewing the steps taken: patient was brought into hospital, admitted with a valid admission order, underwent surgery without complications and deemed safe to discharge the next day. The patient did not spend two midnights in the hospital and both AppriseMD and the hospital agree upon this fact that the patient did not spend two-nights. However, CMS rules at the time of the procedure made an exception to the two-midnight rule for the procedure done in this case. The decision from the ALJ is still pending. |
SOURCES:
- Emanuel, Knicole C.,Esq. “The ALJ Backlog Dissolves – and SMRC Audits Escalate” RAC Monitor April 14, 2021, https://www.racmonitor.com/the-alj-backlog-dissolves-and-smrc-audits-escalate
- United States Senate Congressional Hearing “Creating a More Efficient and Level Playing Field: Audit and Appeals Issues in Medicare” Hearing before the Committee on Finance United States Senate One Hundred Fourteenth Congress First Session S. Hrg. 114-259 https://www.govinfo.gov/content/pkg/CHRG-114shrg20035/html/CHRG-114shrg20035.htm
- HHS https://www.hhs.gov/about/agencies/omha/the-appeals-process/index.html
- HHS https://www.hhs.gov/about/agencies/omha/about/index.html
- Herman, Bob, “Hospitals rake in $1.3 billion from Medicare appeals settlements” June 12, 2015, Modern Healthcare https://www.modernhealthcare.com/article/20150612/NEWS/150619958/hospitals-rake-in-1-3-billion-from-medicare-appeals-settlements